Diagnosis
There is little agreement when it comes to how PCOS is diagnosed. Most physicians will consider this diagnosis after making sure you do not have other conditions such as Cushing's disease (overactive adrenal gland), thyroid problems, congenital adrenal hyperplasia or increased prolactin production by the pituitary gland. Ovaries or PAO).
TSH, 17-hydroxyprogesterone, prolactin and a dexamethasone suppression test may be advisable. After reviewing your medical history, your physicians will determine which tests are necessary. If you have irregular or absent menstrual periods, clues from the physical exam will be considered next.
Your height and weight will be noted along with any increase facial or body hair or loss of scalp hair, acne and acanthosis nigricans (a discoloration of the skin under the arms, breasts and in the groin).
Elevated androgen levels (male hormones) androstenedione, DHEAS or testosterone confirm the diagnosis. A fasting insulin and glucose level will be obtained. Many physicians tell their patients that insulin values are normal, when in fact the value indicates that insulin may be playing a role in stimulating the development of PCOS. Most labs report levels less than 25-30 mIU/ml as normal, while in fact, levels over 10miu/ml on a fasting blood sample suggests that PCOS may be related to hyperinsulinism.
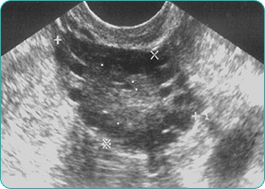
As women with polycystic ovary syndrome may be a greater risk for other medical conditions, testing for blood lipids and diabetes may also be requested. A transvaginal sonar usually showed the poli-follicular appearance of the ovaries [see picture].




